Abstract
Hyperuricaemia (increased serum urate concentration) occurs mainly in higher primates, including in humans, because of inactivation of the gene encoding uricase during primate evolution. Individuals with hyperuricaemia might develop gout — a painful inflammatory arthritis caused by monosodium urate crystal deposition in articular structures. Hyperuricaemia is also associated with common chronic diseases, including hypertension, chronic kidney disease, type 2 diabetes and cardiovascular disease. Many mouse models have been developed to investigate the causal mechanisms for hyperuricaemia. These models are highly diverse and can be divided into two broad categories: mice with genetic modifications (genetically induced models) and mice exposed to certain environmental factors (environmentally induced models; for example, pharmaceutical or dietary induction). This Review provides an overview of the mouse models of hyperuricaemia and the relevance of these models to human hyperuricaemia, with an emphasis on those models generated through genetic modifications. The challenges in developing and comparing mouse models of hyperuricaemia and future research directions are also outlined.
Key points
-
Hyperuricaemia occurs mainly in higher primates, including in humans, primarily owing to inactivation of the uricase gene during primate evolution, which resulted in subsequent evolution of human-specific physiology to tolerate this inactivation.
-
Mouse models of hyperuricaemia have been widely used to provide valuable insights into urate biology but do not yet reliably and consistently simulate the urate-mediated hyperuricaemia that occurs in humans.
-
Such models are potentially valuable resources for dissecting the mechanisms underlying hyperuricaemia as well as the progression from hyperuricaemia to gout and associated comorbidities.
-
A key challenge is to develop uricase-disabled model mice that can survive with increased urate levels and remain healthy and fertile.
-
Community-wide efforts are needed to reach consensus about the definition of hyperuricaemia in mice, to develop protocols for generating suitable models of hyperuricaemia and to adhere to a standard protocol for urate measurements.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dalbeth, N., Merriman, T. R. & Stamp, L. K. Gout. Lancet 388, 2039–2052 (2016).
Ichida, K. et al. Decreased extra-renal urate excretion is a common cause of hyperuricemia. Nat. Commun. 3, 764 (2012). The investigators in this study generate Abcg2 -knockout mice that have increased urate concentrations and reduced gut excretion of urate. The renal excretion of urate is increased in these mice owing to overload of renal urate-handling machinery.
Dalbeth N. et al. Relationship between serum urate concentration and clinically evidence incident gout: an individual participant data analysis. Ann. Rheum. Dis. 77, 1048–1052 (2018).
Bhole, V., Choi, J. W., Kim, S. W., de Vera, M. & Choi, H. Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am. J. Med. 123, 957–961 (2010).
Borghi, C. et al. Serum uric acid and the risk of cardiovascular and renal disease. J. Hypertension 33, 1729–1741 (2015).
Kuo, C. F., Grainge, M. J., Zhang, W. & Doherty, M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 11, 649–662 (2015).
Zhu, Y., Pandya, B. J. & Choi, H. K. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 63, 3136–3141 (2011).
Miao, Z. et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J. Rheumatol. 35, 1859–1864 (2008).
Robinson, P. C., Taylor, W. J. & Merriman, T. R. Systematic review of the prevalence of gout and hyperuricaemia in Australia. Intern. Med. J. 42, 997–1007 (2012).
Chen-Xu, M., Yokose, C., Rai, S. K., Pillinger, M. H. & Choi, H. K. Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the National Health and Nutrition Examination Survey 2007–2016. Arthritis Rheumatol. https://doi.org/10.1002/art.40807 (2019).
Alvarez-Lario, B. & Macarron-Vicente, J. Uric acid and evolution. Rheumatology 49, 2010–2015 (2010).
Friedman, T. B., Polanco, G. E., Appold, J. C. & Mayle, J. E. On the loss of uricolytic activity during primate evolution—I. Silencing of urate oxidase in a hominoid ancestor. Comp. Biochem. Physiol. B 81, 653–659 (1985).
Oda, M., Satta, Y., Takenaka, O. & Takahata, N. Loss of urate oxidase activity in hominoids and its evolutionary implications. Mol. Biol. Evol. 19, 640–653 (2002).
Wu, X. et al. Hyperuricemia and urate nephropathy in urate oxidase-deficient mice. Proc. Natl Acad. Sci. USA 91, 742–746 (1994). This article is the first report of a uricase - knockout mouse, which was developed using ESC-targeting technology. The mice have increased urate concentrations and are viable and fertile, but the mice also have a high mortality owing to severe nephropathy.
Ames, B. N., Cathcart, R., Schwiers, E. & Hochstein, P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc. Natl Acad. Sci. USA 78, 6858–6862 (1981).
Chen, X. et al. Disrupted and transgenic urate oxidase alter urate and dopaminergic neurodegeneration. Proc. Natl Acad. Sci. USA 110, 300–305 (2013).
Major, T. J., Dalbeth, N., Stahl, E. A. & Merriman, T. R. An update on the genetics of hyperuricaemia and gout. Nat. Rev. Rheumatol. 14, 341–353 (2018).
Merriman, T. R. An update on the genetic architecture of hyperuricemia and gout. Arthritis Res. Ther. 17, 98 (2015).
Kanai, M. et al. Genetic analysis of quantitative traits in the Japanese population links cell types to complex human diseases. Nat. Genet. 50, 390–400 (2018).
Köttgen, A. et al. Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat. Genet. 45, 145–154 (2013). This seminal GWAS identifies ~30 loci that are reproducibly associated with serum urate concentration in European individuals.
Nakatochi, M. et al. Genome-wide meta-analysis identifies multiple novel loci associated with serum uric acid levels in Japanese individuals. Commun. Biol. 2, 115 (2019).
Cleophas, M. C. et al. ABCG2 polymorphisms in gout: insights into disease susceptibility and treatment approaches. Pharmacogenomics Pers. Med. 10, 129–142 (2017).
Ketharnathan, S. et al. A non-coding genetic variant maximally associated with serum urate levels is functionally linked to HNF4A-dependent PDZK1 expression. Hum. Mol. Genet. 27, 3964–3973 (2018).
Chhana, A., Lee, G. & Dalbeth, N. Factors influencing the crystallization of monosodium urate: a systematic literature review. BMC Musculoskelet. Disord. 16, 296 (2015).
Lu, J. et al. Knockout of the urate oxidase gene provides a stable mouse model of hyperuricemia associated with metabolic disorders. Kidney Int. 93, 69–80 (2018). This study develops a uricase-deficient mouse line. The mice have increased serum urate concentrations, which are associated with the development of metabolic comorbidities, suggesting that these mice could be used as a model of hyperuricaemia-associated metabolic syndrome.
Cook, S. A. et al. Mouse paracentric inversion In(3)55Rk mutates the urate oxidase gene. Cytogenet. Cell Genet. 93, 77–82 (2001).
Vitart, V. et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat. Genet. 40, 437–442 (2008).
Caulfield, M. J. et al. SLC2A9 is a high-capacity urate transporter in humans. PLOS Med. 5, e197 (2008).
Preitner, F. et al. Glut9 is a major regulator of urate homeostasis and its genetic inactivation induces hyperuricosuria and urate nephropathy. Proc. Natl Acad. Sci. USA 106, 15501–15506 (2009). The investigators in this study generate Slc2a9 -knockout mice that have moderately increased urate concentrations. Unexpectedly, the mice do not develop urate nephropathy or structural abnormalities in the kidneys.
Preitner, F. et al. Urate-induced acute renal failure and chronic inflammation in liver-specific Glut9 knockout mice. Am. J. Physiol. Renal Physiol. 305, F786–F795 (2013).
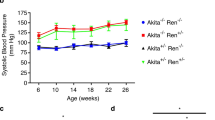
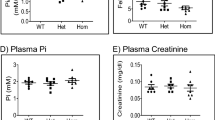
Preitner, F. et al. No development of hypertension in the hyperuricemic liver-Glut9 knockout mouse. Kidney Int. 87, 940–947 (2015).
DeBosch, B. J., Kluth, O., Fujiwara, H., Schurmann, A. & Moley, K. Early-onset metabolic syndrome in mice lacking the intestinal uric acid transporter SLC2A9. Nat. Commun. 5, 4642 (2014). The researchers of this study develop gut-enterocyte-specific Slc2a9 -knockout mice that have moderately increased urate concentrations and metabolic syndrome (including spontaneous hypertension, dyslipidaemia and elevated body fat). These mice might be suitable as a model of hyperuricaemia-associated metabolic syndrome.
Auberson, M. et al. SLC2A9 (GLUT9) mediates urate reabsorption in the mouse kidney. Pflugers Archiv. 470, 1739–1751 (2018).
Dinour, D. et al. Homozygous mutations cause severe renal hypouricemia. J. Am. Soc. Nephrol. 21, 64–72 (2010).
Johnson, R. J. et al. Hyperuricemia, acute and chronic kidney disease, hypertension and cardiovascular disease: report of a scientific workshop organized by the National Kidney Foundation. Am. J. Kidney Dis. 71, 851–865 (2018).
Johnson, R. J., Merriman, T. & Lanaspa, M. A. Causal or noncausal relationship of uric acid with diabetes. Diabetes 64, 2720–2722 (2015).
Robinson, P. C., Choi, H. K., Do, R. & Merriman, T. R. Insight into rheumatological cause and effect through the use of Mendelian randomization. Nat. Rev. Rheumatol. 12, 486–496 (2016).
Li, X. et al. Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. BMJ 357, j2376 (2017).
Woodward, O. M. et al. Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc. Natl Acad. Sci. USA 106, 10338–10342 (2009).
Matsuo, H. et al. Common defects of ABCG2, a high-capacity urate exporter, cause gout: a function-based genetic analysis in a Japanese population. Sci. Transl Med. 1, 5ra11 (2009).
Takada, T. et al. ABCG2 dysfunction increases serum uric acid by decreased intestinal urate excretion. Nucleosides Nucleotides Nucleic Acids 33, 275–281 (2014).
Fridovich, I. The competitive inhibition of uricase by oxonate and by related derivatives of s-Triazines. J. Biol. Chem. 240, 2491–2494 (1965).
Matsuo, H. et al. ABCG2 dysfunction causes hyperuricemia due to both renal urate underexcretion and renal urate overload. Sci. Rep. 4, 3755 (2014).
Kannangara, D. R. et al. Hyperuricaemia: contributions of urate transporter ABCG2 and the fractional renal clearance of urate. Ann. Rheum. Dis. 75, 1363–1365 (2015).
Hoque, K. M. & Woodward, O. M. New mouse model of gout risk variant, ABCG2 Q141K, reveals unexpectedly severe molecular and functional defect in ABCG2 mediated intestinal uric acid secretion [abstract 2898]. Arthritis Rheumatol. 69 (Suppl. 10), 4187 (2017).
Sulem, P. et al. Identification of low-frequency variants associated with gout and serum uric acid levels. Nat. Genet. 43, 1127–1130 (2011).
Tanner, C. et al. Population-specific resequencing associates the ATP-binding cassette subfamily C member 4 gene with gout in New Zealand Maori and Pacific men. Arthritis Rheumatol. 69, 1461–1469 (2017).
Eraly, S. A. et al. Multiple organic anion transporters contribute to net renal excretion of uric acid. Physiol. Genomics 33, 180–192 (2008).
Hosoyamada, M. et al. Establishment and analysis of SLC22A12 (URAT1) knockout mouse. Nucleosides Nucleotides Nucleic Acids 29, 314–320 (2010). In this study, Slc22a12 -knockout mice are generated that have considerably increased serum concentrations of urate, although the fractional excretion of urate in the knockout mice is higher than that of wild-type mice.
Hosoyamada, M. et al. Urat1-Uox double knockout mice are experimental animal models of renal hypouricemia and exercise-induced acute kidney injury. Nucleosides Nucleotides Nucleic Acids 35, 543–549 (2016).
Kocher, O., Pal, R., Roberts, M., Cirovic, C. & Gilchrist, A. Targeted disruption of the PDZK1 gene by homologous recombination. Mol. Cell. Biol. 23, 1175–1180 (2003).
Hillesheim, J. et al. Down regulation of small intestinal ion transport in PDZK1- (CAP70/NHERF3) deficient mice. Pflugers Arch. 454, 575–586 (2007).
Charkoftaki, G. et al. Transcriptomic analysis and plasma metabolomics in Aldh16a1-null mice reveals a potential role of ALDH16A1 in renal function. Chem. Biol. Interact. 276, 15–22 (2017).
Lin, Z. P. et al. Disruption of cAMP and prostaglandin E2 transport by multidrug resistance protein 4 deficiency alters cAMP-mediated signaling and nociceptive response. Mol. Pharmacol. 73, 243–251 (2008).
Dankers, A. C. A. et al. Hyperuricemia influences tryptophan metabolism via inhibition of multidrug resistance protein 4 (MRP4) and breast cancer resistance protein (BCRP). Biochim. Biophys. Acta 1832, 1715–1722 (2013).
Aziz, A., Soucie, E., Sarrazin, S. & Sieweke, M. H. MafB/c-Maf deficiency enables self-renewal of differentiated functional macrophages. Science 326, 867–871 (2009).
Katsuoka, F., Yamazaki, H. & Yamamoto, M. Small Maf deficiency recapitulates the liver phenotypes of Nrf1- and Nrf2-deficient mice. Genes Cells 21, 1309–1319 (2016).
Lyon, M. F. et al. A dominant mutation within the DNA-binding domain of the bZIP transcription factor Maf causes murine cataract and results in selective alteration in DNA binding. Hum. Mol. Genet. 12, 585–594 (2003).
Kelley, W. N., Rosenbloom, F. M., Henderson, J. F. & Seegmiller, J. E. A specific enzyme defect in gout associated with overproduction of uric acid. Proc. Natl Acad. Sci. USA 57, 1735–1739 (1967).
Zennaro, C. et al. The renal phenotype of allopurinol-treated HPRT-deficient mouse. PLOS ONE 12, e0173512 (2017).
Ma, L. et al. Point mutation in D8C domain of Tamm-Horsfall protein/uromodulin in transgenic mice causes progressive renal damage and hyperuricemia. PLOS ONE 12, e0186769 (2017).
Stevenson, W. S. et al. Deficiency of 5-hydroxyisourate hydrolase causes hepatomegaly and hepatocellular carcinoma in mice. Proc. Natl Acad. Sci. USA 107, 16625–16630 (2010).
Baey, C., Yang, J., Ronchese, F. & Harper, J. L. Hyperuricaemic Urah Plt2/Plt2 mice show altered T cell proliferation and defective tumor immunity after local immunotherapy with Poly I:C. PLOS ONE 13, e0206827 (2018).
Wu, X. H. et al. Riparoside B and timosaponin J, two steroidal glycosides from Smilax riparia, resist to hyperuricemia based on URAT1 in hyperuricemic mice. Phytomedicine 21, 1196–1201 (2014).
Wang, M. X., Liu, Y. L., Yang, Y., Zhang, D. M. & Kong, L. D. Nuciferine restores potassium oxonate-induced hyperuricemia and kidney inflammation in mice. Eur. J. Pharmacol. 747, 59–70 (2015).
Wang, M., Zhao, J., Zhang, N. & Chen, J. Astilbin improves potassium oxonate-induced hyperuricemia and kidney injury through regulating oxidative stress and inflammation response in mice. Biomed. Pharmacother. 83, 975–988 (2016).
Chen, G., Tan, M. L., Li, K. K., Leung, P. C. & Ko, C. H. Green tea polyphenols decreases uric acid level through xanthine oxidase and renal urate transporters in hyperuricemic mice. J. Ethnopharmacol. 175, 14–20 (2015).
Watanabe, T., Tomioka, N. H., Watanabe, S., Tsuchiya, M. & Hosoyamada, M. False in vitro and in vivo elevations of uric acid levels in mouse blood. Nucleosides Nucleotides Nucleic Acids 33, 192–198 (2014). This study highlights the extreme variability in mouse urate concentrations measured across different studies. There is a 19-fold difference in urate concentrations between live and dead mice sampled for blood urate measurements.
Li, J. M., Zhang, X., Wang, X., Xie, Y. C. & Kong, L. D. Protective effects of cortex fraxini coumarines against oxonate-induced hyperuricemia and renal dysfunction in mice. Eur. J. Pharmacol. 666, 196–204 (2011).
Hu, Q. H., Zhang, X., Wang, X., Jiao, R. Q. & Kong, L. D. Quercetin regulates organic ion transporter and uromodulin expression and improves renal function in hyperuricemic mice. Eur. J. Nutr. 51, 593–606 (2012).
Liu, Y. L. et al. Betaine reduces serum uric acid levels and improves kidney function in hyperuricemic mice. Planta Med. 80, 39–47 (2014).
Yong, T. et al. Actions of water extract from Cordyceps militaris in hyperuricemic mice induced by potassium oxonate combined with hypoxanthine. J. Ethnopharmacol. 194, 403–411 (2016).
Sun, W. F. et al. MicroRNA expression patterns of the kidney in hyperuricemia mice treated with Xiezhuo Chubi Decoction. Chin. J. Integr. Med. 17, 35–42 (2011).
Xu, C. et al. Xanthine oxidase in non-alcoholic fatty liver disease and hyperuricemia: one stone hits two birds. J. Hepatol. 62, 1412–1419 (2015).
Nakatsu, Y. et al. The xanthine oxidase inhibitor febuxostat suppresses development of nonalcoholic steatohepatitis in a rodent model. Am. J. Physiol. Gastrointest. Liver Physiol. 309, G42–G51 (2015).
Bakker, P. J. et al. Nlrp3 is a key modulator of diet-induced nephropathy and renal cholesterol accumulation. Kidney Int. 85, 1112–1122 (2014).
Mutel, E. et al. Targeted deletion of liver glucose-6 phosphatase mimics glycogen storage disease type 1a including development of multiple adenomas. J. Hepatol. 54, 529–537 (2011).
Ito, T. et al. Glomerular changes in the KK-Ay/Ta mouse: a possible model for human type 2 diabetic nephropathy. Nephrology 11, 29–35 (2006).
Adachi, S. I., Yoshizawa, F. & Yagasaki, K. Hyperuricemia in type 2 diabetic model KK-Ay/Ta mice: a potent animal model with positive correlation between insulin resistance and plasma high uric acid levels. BMC Res. Notes 10, 577 (2017).
Baldwin, W. et al. Hyperuricemia as a mediator of the proinflammatory endocrine imbalance in the adipose tissue in a murine model of the metabolic syndrome. Diabetes 60, 1258–1269 (2011).
Shaw, O. M., Pool, B., Dalbeth, N. & Harper, J. L. The effect of diet-induced obesity on the inflammatory phenotype of non-adipose-resident macrophages in an in vivo model of gout. Rheumatology 53, 1901–1905 (2014).
Marchetti, C. et al. NLRP3 inflammasome inhibitor OLT1177 suppresses joint inflammation in murine models of acute arthritis. Arthritis Res. Ther. 20, 169 (2018).
Amaral, F. A. et al. Transmembrane TNF-α is sufficient for articular inflammation and hypernociception in a mouse model of gout. Eur. J. Immunol. 46, 204–211 (2016).
Liu-Bryan, R., Scott, P., Sydlaske, A., Rose, D. M. & Terkeltaub, R. Innate immunity conferred by Toll-like receptors 2 and 4 and myeloid differentiation factor 88 expression is pivotal to monosodium urate monohydrate crystal-induced inflammation. Arthritis Rheum. 52, 2936–2946 (2005).
Lee, Y. M., Shon, E. J., Kim, O. S. & Kim, D. S. Effects of Mollugo pentaphylla extract on monosodium urate crystal-induced gouty arthritis in mice. BMC Complement. Altern. Med. 17, 447 (2017).
Cumpelik, A., Ankli, B., Zecher, D. & Schifferli, J. A. Neutrophil microvesicles resolve gout by inhibiting C5a-mediated priming of the inflammasome. Ann. Rheum. Dis. 75, 1236–1245 (2016).
Crisan, T. O. et al. Soluble uric acid primes TLR-induced proinflammatory cytokine production by human primary cells via inhibition of IL-1Ra. Ann. Rheum. Dis. 75, 755–762 (2016).
Mazzali, M. et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 38, 1101–1106 (2001).
Su, Q. et al. Hypouricemic and nephroprotective effects of an active fraction from Polyrhachis Vicina Roger on potassium oxonate-induced hyperuricemia in rats. Kidney Blood Press. Res. 43, 220–233 (2018).
Liu, X., Chen, R., Shang, Y., Jiao, B. & Huang, C. Lithospermic acid as a novel xanthine oxidase inhibitor has anti-inflammatory and hypouricemic effects in rats. Chem. Biol. Interact. 176, 137–142 (2008).
Leask, M. et al. Functional urate-associated genetic variants influence expression of lincRNAs LINC01229 and MAFTRR. Front. Genet. 9, 733 (2018).
Zhang, Y., Li, Q., Wang, F. & Xing, C. A zebrafish (danio rerio) model for high-throughput screening food and drugs with uric acid-lowering activity. Biochem. Biophys. Res. Commun. 508, 494–498 (2019).
Marchetti, M. et al. Catalysis and structure of zebrafish urate oxidase provide insights into the origin of hyperuricemia in hominoids. Sci. Rep. 6, 38302 (2016).
Hall, C. J. et al. Blocking fatty acid-fueled mROS production within macrophages alleviates acute gouty inflammation. J. Clin. Invest. 128, 1752–1771 (2018).
Remy, C., Richert, D. A. & Westerfeld, W. W. The determination of xanthine dehydrogenase in chicken tissues. J. Biol. Chem. 192, 649–657 (1951).
Ejaz, S., Kim, B. S. & Lim, C. W. Gout induced by intoxication of sodium bicarbonate in Korean native broilers. Drug Chem. Toxicol. 28, 245–261 (2005).
Poffers, J., Lumeij, J. T., Timmermans-Sprang, E. P. & Redig, P. T. Further studies on the use of allopurinol to reduce plasma uric acid concentrations in the Red-tailed Hawk (Buteo jamaicensis) hyperuricaemic model. Avian Pathol. 31, 567–572 (2002).
Lin, Z., Zhang, B., Liu, X., Jin, R. & Zhu, W. Effects of chicory inulin on serum metabolites of uric acid, lipids, glucose, and abdominal fat deposition in quails induced by purine-rich diets. J. Med. Food 17, 1214–1221 (2014).
Zhang, X. H. et al. Molecular characterization, balancing selection, and genomic organization of the tree shrew (Tupaia belangeri) MHC class I gene. Gene 522, 147–155 (2013).
Tang, D. H. et al. Potassium oxonate induces acute hyperuricemia in the tree shrew (tupaia belangeri chinensis). Exp. Anim. 66, 209–216 (2017).
Szczurek, P. et al. Oral uricase eliminates blood uric acid in the hyperuricemic pig model. PLOS ONE 12, e0179195 (2017).
Bannasch, D. et al. Mutations in the SLC2A9 gene cause hyperuricosuria and hyperuricemia in the dog. PLOS Genet. 4, e1000246 (2008).
Rothschild, B. M., Tanke, D. & Carpenter, K. Tyrannosaurs suffered from gout. Nature 387, 357 (1997).
Ammerman, L. E. Resurrecting Tyrannosaurus rex. Thesis, Baylor Univ. Texas (2016).
Fatima, T. et al. The relationship between ferritin and urate levels and risk of gout. Arthritis Res. Ther. 20, 179 (2018).
Topless, R. K. et al. Association of SLC2A9 genotype with phenotypic variability of serum urate in pre-menopausal women. Front. Genet. 6, 313 (2015).
Okada, Y. et al. Meta-analysis identifies multiple loci associated with kidney function-related traits in east Asian populations. Nat. Genet. 44, 904–909 (2012).
Kratzer, J. T. et al. Evolutionary history and metabolic insights of ancient mammalian uricases. Proc. Natl Acad. Sci. USA 111, 3763–3768 (2014).
Tan, P. K., Farrar, J. E., Gaucher, E. A. & Miner, J. N. Coevolution of URAT1 and uricase during primate evolution: implications for serum urate homeostasis and gout. Mol. Bio. Evol. 33, 2193–2200 (2016).
Kelly, S. J. et al. Diabetes insipidus in uricase-deficient mice: a model for evaluating therapy with poly(ethylene glycol)-modified uricase. J. Am. Soc. Nephrol. 12, 1001–1009 (2001).
Zhang, F., Wen, Y. & Guo, X. CRISPR/Cas9 for genome editing: progress, implications and challenges. Hum. Mol. Genet. 23, R40–R46 (2014).
Cleveland, B. M., Leonard, S. S., Klandorf, H. & Blemings, K. P. Urate oxidase knockdown decreases oxidative stress in a murine hepatic cell line. Oxid. Med. Cell. Longev. 2, 93–98 (2009).
Silva, A. J. et al. Mutant mice and neuroscience: recommendations concerning genetic background. Neuron 19, 755–759 (1997).
Montagutelli, X. Effect of the genetic background on the phenotype of mouse mutations. J. Am. Soc. Nephrol. 11, S101–S105 (2000).
Dalbeth, N. et al. Relationship between serum urate concentration and clinically evident incident gout: an individual participant data analysis. Ann. Rheum. Dis. 77, 1048–1052 (2018).
Terkeltaub, R. What makes gouty inflammation so variable? BMC Med. 15, 158 (2017).
Schauer, C. et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat. Med. 20, 511–517 (2014).
Pascual, E., Addadi, L., Andres, M. & Sivera, F. Mechanisms of crystal formation in gout-a structural approach. Nat. Rev. Rheumatol. 11, 725–730 (2015).
Mandal, A. K. & Mount, D. B. The molecular physiology of uric acid homeostasis. Annu. Rev. Physiol. 77, 323–345 (2015).
Sutin, A. R. et al. Impulsivity is associated with uric acid: evidence from humans and mice. Biol. Psychiatry 75, 31–37 (2014).
Lu, J. et al. Urate-lowering therapy alleviates atherosclerosis inflammatory response factors and neointimal lesions in a mouse model of induced carotid atherosclerosis. FEBS J. 286, 1346–1359 (2019).
Lizio, M. et al. Gateways to the FANTOM5 promoter level mammalian expression atlas. Genome Biol. 16, 22 (2015).
RIKEN. Functional annotation of the mammalian genome. FANTOM http://fantom.gsc.riken.jp/ (2014).
The Scripps Research Institute. BioGPS. BioGPS http://biogps.org (2019).
Wu, C., Jin, X., Tsueng, G., Afrasiabi, C. & Su, A. I. BioGPS: building your own mash-up of gene annotations and expression profiles. Nucl. Acids Res. 44, D313–D316 (2016).
Hruz, T. et al. Genevestigator V3: a reference expression database for the meta-analysis of transcriptomes. Adv. Bioinformatics 2008, 420747 (2008).
Nebion. Genevestigator. Geneinvestigator https://genevestigator.com/gv/ (2018).
Acknowledgements
The authors thank S. Robertson and the Clinical Genetics Group in the University of Otago, Dunedin, New Zealand, for their valuable discussions of this Review. J.L. is grateful for the support of the Departments of Women’s and Children’s Health, Biochemistry and Pathology, University of Otago. W.-H.W. is funded by Cure Kids NZ and the University of Otago.
Reviewer information
Nature Reviews Rheumatology thanks H. -K. Ea and F. Lioté for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
J.L., C.L. and W.-H.W. researched data for the article. N.D., T.R.M. and W.-H.W. contributed to discussion of content. J.L., N.D., H.Y., T.R.M. and W.-H.W. contributed to writing the article, and all authors reviewed and edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
N.D. declares that she has received research grant funding from Amgen and AstraZeneca; speaker fees from AbbVie, Janssen and Pfizer; and consulting fees from AstraZeneca, Horizon and Kowa. T.R.M. declares he has received research grant funding from Ardea Biosciences and Ironwood Pharmaceuticals and has received consulting fees from Ironwood Pharmaceuticals. The other authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Mendelian ratios
-
The expected ratios of genotypes at a locus observed in offspring under Mendel’s law of independent assortment; if one allele is embryonically lethal, the ratio will be skewed.
- Mendelian randomization
-
The use of genetic variation in genes of known function to examine the causal effect of an exposure on disease in observational studies.
- Pseudogenization
-
The process of generating a pseudogene, which is a gene that has DNA segments related to a real gene but has lost some or all functionality during evolution.
- Congenic
-
A congenic mouse strain has a defined segment from a donor strain introduced into its genome.
Rights and permissions
About this article
Cite this article
Lu, J., Dalbeth, N., Yin, H. et al. Mouse models for human hyperuricaemia: a critical review. Nat Rev Rheumatol 15, 413–426 (2019). https://doi.org/10.1038/s41584-019-0222-x
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-019-0222-x
This article is cited by
-
Lactobacillus rhamnosus GG ameliorates hyperuricemia in a novel model
npj Biofilms and Microbiomes (2024)
-
Platinum nanoparticles confined in metal–organic frameworks as excellent peroxidase-like nanozymes for detection of uric acid
Analytical and Bioanalytical Chemistry (2023)
-
Mechanistic insights of soluble uric acid-induced insulin resistance: Insulin signaling and beyond
Reviews in Endocrine and Metabolic Disorders (2023)
-
CDER167, a dual inhibitor of URAT1 and GLUT9, is a novel and potent uricosuric candidate for the treatment of hyperuricemia
Acta Pharmacologica Sinica (2022)
-
The regulation effect of GLUT9/SLC2A9 on intrahepatic uric acid level and metabolic associated fatty liver disease
Hepatology International (2022)