Sharing treatment protocols leads to better outcomes

Chronic back pain that persists beyond 12 weeks can be challenging to diagnose and treat. Because it can be so complex, the most effective care involves a multidisciplinary, multimodal approach that considers the physical and psychological aspects of the pain.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These patients with chronic back pain can benefit from the combined expertise of specialists from different disciplines. This thinking was the catalyst for collaboration between back pain specialists in Cleveland Clinic’s Department of Pain Management and the Center for Spine Health, which is part of Cleveland Clinic’s Neurological Institute.
Six interventional pain specialists from the Pain Management Department are now integrated with the Center. The sharing of specialized knowledge, perspectives, diagnostic and treatment techniques, and interventional methods is improving outcomes for patients, including many who present with severe problems.
“We have wanted to collaborate for many years,” says Richard Rosenquist, MD, Chair of Pain Management. “This improves access and provides a broader range of services to our Cleveland Clinic back pain patients. It also gives our physicians the ability to learn from each other and to collaborate at a leadership level.”
The Center for Spine Health includes the expertise of specialists in orthopaedic spine surgery, neurosurgery, physical medicine and rehabilitation, rheumatology, and primary care to offer the most innovative and effective medical and surgical treatments.
Cleveland Clinic physicians who treat chronic back pain will, whenever possible, prescribe nonsurgical options first. While some patients do benefit from surgery, the goal for every patient is to provide optimal symptom relief as conservatively as possible.
In addition to treating patients with medication, back pain specialists in Pain Management are skilled in a wide range of interventional techniques, including:
“But the first step is always to understand why this person is having back pain,” says Paul Shin, MD, a pain management specialist now collaborating in the Spine Center. The initial consultation includes a thorough medical history, a physical exam, and imaging and blood work as needed. Causes can range from musculoskeletal or ligamental disorders to problems involving arthritis, the disks, nerves, joints or autoimmune issues. “There’s one diagnosis — low back pain — but there can be 10 different things going on. Most of the time it’s a combination of several factors and we are looking for the main source of the cause,” he says.
Dr. Shin is a strong believer in beginning treatment for most patients with physical therapy. “The stronger the muscles and ligaments surrounding the spine, the better, so ultimately strengthening the spine may not only keep one away from injections or surgery, it also reduces the chances of recurring back pain. For this reason, no matter what the diagnosis may be, physical therapy is usually a good first option.”
The Pain Management Department has referred many patients to Cleveland Clinic’s population health management program called Back on TREK (Transform Restore Empower Knowledge). It was developed by the Center for Spine Health for patients whose lower back pain has lasted for three or more months.
The 12-week program also uses a multidisciplinary approach to promote functional recovery and to empower patients. Patients participate in individual and group physical therapy and behavioral health sessions with a pain psychologist.
A recent study of individuals who completed Back on TREK revealed significantly better outcomes and quality of life improvements compared to a control that received standard physical therapy, reports pain psychologist Sara Davin, PsyD, MPH.
She believes that success stems partly from the group interaction. “Patients with back pain often feel isolated and misunderstood. This program addresses that,” she says.
Through individual cognitive behavioral therapy, patients also learn to manage the emotional aspects of their pain. “Fear, anger and hopelessness are like putting gasoline on the fire,” she says. “We teach people how to interpret their pain, change the way they think, and handle their emotions through behaviors they adopt in response to pain.” This cognitive approach also works well both pre- and postoperatively for patients who undergo spine surgery, she adds.
Patients continue to follow up with their pain management provider, she stresses. “It can be hard to get buy-in from a patient unless they also have a medical doctor who helps to validate that their pain is real.”
Though physical and cognitive behavioral therapy are very helpful, “I always tell people that they’re in the pain management doctor’s office because their condition is complicated, and it’s unlikely that one thing is going to solve the problem,” adds Dr. Shin. “It’s usually going to be a combination of things that helps them get better.”

Program enhances cooperation between traditional and non-pharmacologic care

Pain specialists can play a role in identifying surgical candidates

Clinical judgment is foundational to appropriately prescribing

The device is a less invasive alternative for patients who are struggle with chronic pain

The Four Pillar Project provides physicians with evidence-based talking points to quickly identify problem areas and educate patients to optimize important aspects of their health.
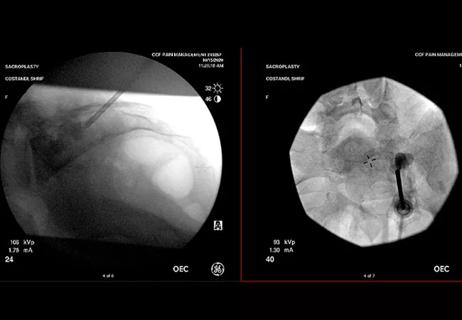
When conservative approaches don’t work, it may be time to turn to sacroplasty

Fourth iteration of the guidelines focuses on high-risk patient identification and evidence on newer drugs

It is a lifestyle commitment that can minimize pain and improve lives